Harnessing AI for Precision Public Health: From Biomedical Knowledge Engineering to Smarter Intervention
In the evolving landscape of learning health systems and AI for precision health, researchers must analyze an overwhelming volume of biomedical data to extract actionable insights. At Columbia University, Harry Reyes Nieva, PhD, set out to make this process more scalable, systematic, and sustainable. His innovative research focuses on refining how biomedical data is acquired, organized, analyzed, and applied—ensuring that AI-driven discoveries lead to real-world improvements in public health.
From Grassroots Advocacy to Global Health Initiatives
His career in biomedical informatics may appear to have begun during his PhD journey at Columbia University, but his real path began much earlier while working on public health initiatives in sub-Saharan Africa, grassroots advocacy in New Haven, and in hospitals
transforming clinical data systems. At the age of 16, Harry entered Yale University as a first-generation college student from a predominantly Puerto Rican neighborhood in Brooklyn, NY. Determined to make an impact on his community, he quickly became involved in Student Health OUTreach (SHOUT), a small student-run initiative aimed at helping uninsured residents of New Haven, Conn., seeking medical care. Eventually, SHOUT would transform into Advanced Strategies for Healthcare Access (ASHA), a full-fledged nonprofit, backed by city leadership and prominent foundations. This early venture began a throughline that still encapsulates much of his work—innovation grounded in meaningful, real-world impact.
After college and a brief time as a New York City public school teacher, Reyes Nieva took these principles to the global stage, joining Harvard’s arm of the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), which aimed to rapidly expand life-saving treatment for people living with HIV/AIDS around the world. During that time, he played an integral role in capacity building efforts in multiple countries and scaling a comprehensive, homegrown electronic health record (EHR) system for HIV/AIDS care in Nigeria—transitioning clinics from handwritten notes to real-time digital records. In this capacity, Reyes Nieva also co-designed quality monitoring dashboards and data-driven point-of-care tools that shaped clinical decisions for patients across the country. This work showed him that technology could drive significant advances in population health if implemented creatively and judiciously.
Catalyzing Systemic Change in Clinical Care and Research Initiatives
After his tenure at PEPFAR, Reyes Nieva deepened his expertise in the Division of General Internal Medicine and Primary Care at Brigham and Women’s Hospital (BWH), working extensively in health services research while simultaneously taking graduate courses in population and international health at the Harvard T.H. Chan School of Public Health and completing a Master of Applied Science at the Johns Hopkins Bloomberg School of Public Health. At BWH, he helped establish a primary care practice-based research network that rapidly garnered institutional recognition for its innovative methods in patient-centered research. One of his most notable successes during this time was advocating for Partners Healthcare (now known as Mass General Brigham) to expand standardized demographic data routinely collected in its EHR. Besides improving patient care, the work set a foundation to support population health research by enhancing data quality and inclusion of important data elements.
Toward Transforming Healthcare and Biomedical Research with AI Initiatives
Motivated to better leverage the tremendous potential of AI and informatics for medicine and public health, Reyes Nieva pursued a PhD at Columbia University’s Department of Biomedical Informatics (DBMI). He was drawn by the program’s strong reputation and identified Noémie Elhadad, now DBMI Chair and Associate Professor, early on as an ideal mentor.
Under Elhadad’s mentorship, Reyes Nieva developed a research agenda that would bridge his extensive real-world experience with more advanced computational

techniques. His PhD work focused on designing AI and informatics-driven approaches that can continuously learn from biomedical literature and real-world healthcare data, with the goal of improving health outcomes for all populations. Reyes Nieva describes his research as “development and application of responsible, human-centered AI to enable learning health systems and support precision public health.”
“Harry addresses multiple challenges in precision public health research, including access to continuously updated real-world data and making sense of the data messiness, especially when it comes from multiple health systems.” Elhadad said. “Harry’s work is so important because it turns that chaos into something we can actually use to learn about our patient population and their patterns of care, make public health decisions, and ultimately improve care. That’s the learning health system Harry envisioned in his thesis.
“What made him the right person for this work wasn’t just his technical skills, but also his deep understanding of public health, his expertise in STIs, and his ability to collaborate across disciplines, in particular with our Infectious Disease collaborators,” she added. “That combination is rare, and it’s what allowed him to take on such a complex problem and deliver something truly impactful.”
His PhD training was supported by prestigious research training fellowships from the National Library of Medicine (NLM) and National Institute of Allergy and Infectious Diseases (NIAID), as well as an Association for Computing Machinery (ACM) Special Interest Group in High Performance Computing (SIGHPC) Computational & Data Science Fellowship. In the final year of his PhD, he was also named a DAAD AInet Fellow for Safety and Security in AI by the German academic exchange service, Deutscher Akademischer Austauschdienst (DAAD), highlighting his early global trajectory as a promising AI scientist.
Transforming Evidence Synthesis in Biomedical Science with AI Initiatives
Reyes Nieva’s dissertation work included creating HDMH Monitor, an innovative AI-driven system designed to mine the vast array of available scientific literature to uncover previously invisible research gaps. First introduced in the high-impact journal Science Advances, this system uses natural language processing, machine learning, and knowledge engineering to systematically identify lesser-studied diseases, populations, and themes among millions of biomedical articles and comparing them to insights drawn from real-world clinical databases and public health reporting—transforming literature review from an overwhelming task to a clear, actionable guide for scientific researchers and policymakers.
“When you have a limited number of articles and you put a group of experts in a room, performing a scoping review and gap analysis requires a substantial amount of effort, but it is feasible,” Reyes Nieva said. “The real challenge is doing this at scale. How do you computationally answer the question, ‘What’s missing?’ when it’s hard enough to characterize what’s actually there?”
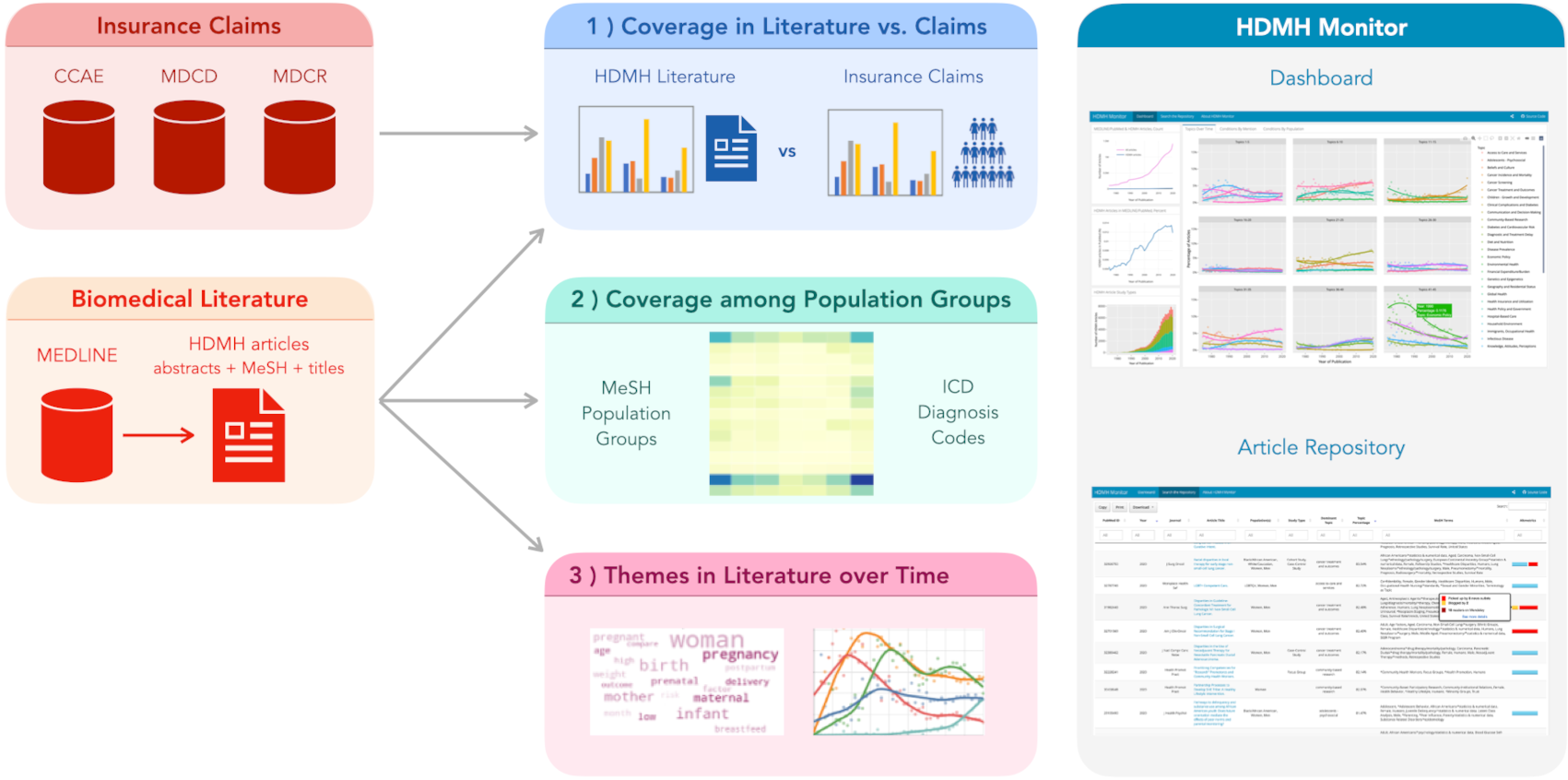
Source: Reyes Nieva H et al. Science Advances. 2024.
Between 1975 and 2020, PubMed’s database grew to nearly 28 million articles, yet individual researchers performing literature searches would not be able to determine which areas had been under-investigated. HDMH Monitor supports this process by systematically mining search results to highlight missing connections or underrepresented topics. This can shape future research directions by revealing key biomedical knowledge gaps. By informing future literature searches to be more precise and efficient, this work provides a powerful tool for researchers, clinicians, and public health experts, ensuring that AI can drive knowledge-seeking and planning across the healthcare landscape.
AI-Driven Subgroup Discovery for Precision Population Health
To further translate large-scale data into targeted decision-making and healthcare interventions, Reyes Nieva also sought to address a critical public health challenge: identifying specific at-risk populations using model-based techniques. Traditional epidemiological methods often rely on broad demographic categories, which can obscure the nuanced ways factors like age, sex, and geography intersect to influence health outcomes.
One of his key research efforts focused on adapting a novel machine learning technique that employs supervised clustering to uncover meaningful patterns in patient data across subpopulation intersections.
“In traditional clustering methods, subgroups of patients are typically identified based on common characteristics, without necessarily considering how these characteristics relate directly to health outcomes,” said Reyes Nieva. “By simultaneously encoding information about a particular outcome of interest, our approach goes a step further to distinguish among only the most important attributes that define those different subpopulations, effectively ensuring we find meaningful, actionable subgroups. Importantly, our technique is capable of discerning differences that would otherwise be missed because it’s just not practical to examine all possible combinations of patient-level factors.”
As an innovative application of AI for precision public health, this represents a key step forward by moving beyond broad population group classifications. This new technique provides a more precise, scalable path to analyze patient data and better target specialized interventions to different subgroups. Critically, there are significant implications that enable clinicians, health systems, and public health agencies to tailor different interventions to those who might benefit most and more effectively allocate resources to achieve better outcomes for everyone.
Fostering Learning Public Health Systems
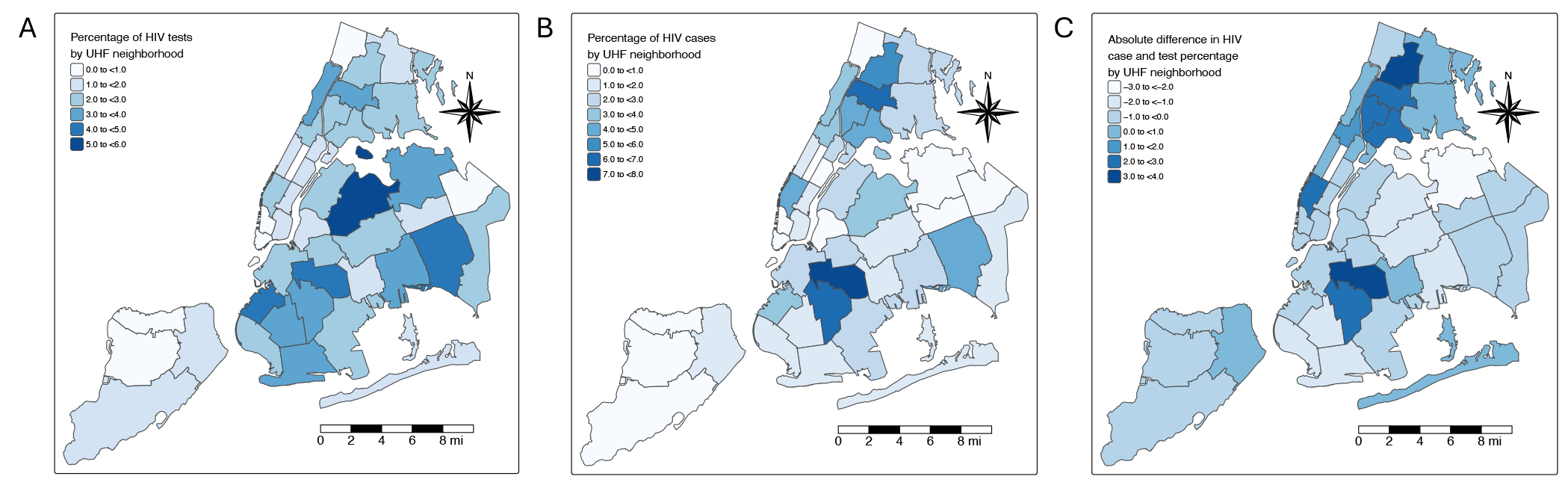
Source: Reyes Nieva H et al. JAMA Network Open. 2025.
In contrast to his model-based approach, another cornerstone of his doctoral research focused on better harnessing and integrating existing sources of data to improve public health surveillance. Recently published in JAMA Network Open, this work specifically leveraged clinical data from health information exchanges and open government data to foster a learning public health system, wherein near real-time data-driven insights are integrated to inform, evaluate, and adapt public health strategies.
“Current public health reporting systems and data infrastructures are highly fragmented and lack timely, comprehensive data, resulting in limited surveillance capacity,” said Reyes Nieva. “Our approach embraces the key hallmarks of infectious disease surveillance in the era of big data —volume, variety, velocity, and value—and operates at a scale commensurate with regional public health agencies while enabling analyses not typically possible with traditional public health reporting.”
By analyzing harmonized EHRs for nearly five million patients across multiple major New York City healthcare systems, Reyes Nieva and colleagues identified critical gaps in routine screening practices and resource allocation for multiple infectious diseases. His work vividly demonstrates how informatics can enable more responsive and precise public health strategies to identify nuanced patterns of disease risk and healthcare needs.
Leveraging OMOP for Scalable Data Integration
To perform his work on learning public health systems, Reyes Nieva first had to address the complex task of harmonizing EHR data across multiple healthcare institutions. Fortunately, a globally recognized standard—coordinated within Columbia’s Department of Biomedical Informatics—provided the necessary framework. The Observational Medical Outcomes Partnership (OMOP) Common Data Model, which underpins all global research within the Columbia-led Observational Health Data Sciences and Informatics (OHDSI) community, standardized the EHR data for his large-scale analysis.
This foundational tool was instrumental in Reyes Nieva’s research, just as it has been for the 4,200+ collaborators within OHDSI. Looking back, he wishes he had leveraged OHDSI’s resources earlier in his research journey at Columbia, but now he is committed to helping others benefit from its tools, methods, and global research network. Recently, he took on a co-lead role in the Early-Stage Researchers workgroup—one step in what he hopes will be a long career of mentorship in academia.
“I love mentorship,” he said. “I’ve mentored prior to and throughout my PhD. It has always been important to me. The research is first and foremost, but a big part of the research is mentoring that next group of trainees. Engaging them early on in their careers and ensuring they are trained in OHDSI’s collaborative frameworks and open standards will also be vital to scaling AI tools effectively across health systems and countries. I’m also eager to expand OHDSI’s reach to regions of the world where OHDSI does not yet have a major presence and where its ability to leapfrog innovation and improvements in care are vitally needed.”
A Global Vision to Bridge AI and Public Good
Looking ahead—with an eye toward eventually leading his own research lab—OHDSI’s global footprint and core values of innovation, reproducibility, community, collaboration, openness, and beneficence are well aligned with Reyes Nieva’s ethos and vision for his future career. Bringing his expertise in AI, biomedical informatics, and public health to bear, his recent appointment as a postdoctoral research scientist at Columbia’s Division of Infectious Diseases positions him strategically to bridge AI innovation with transformative public health action. One of his upcoming collaborations with technical leads in disease surveillance at the World Health Organization illustrates his commitment to applying advanced informatics and AI to strengthen health information systems worldwide. Above all, as Dr. Reyes Nieva remarked, his career is clearly driven by a central guiding principle, “technology achieves its highest purpose when it directly improves human lives.”

