Personalizing Treatment for Chronic Illness:
The Role of AI in Empowering Patients
Chronic illnesses, including cardiovascular, autoimmune, metabolic, and mental health disorders, are the leading cause of disability worldwide and account for 70% of global deaths, according to the World Health Organization. They pose immense challenges for both patients and providers and represent the greatest financial strain on healthcare systems.
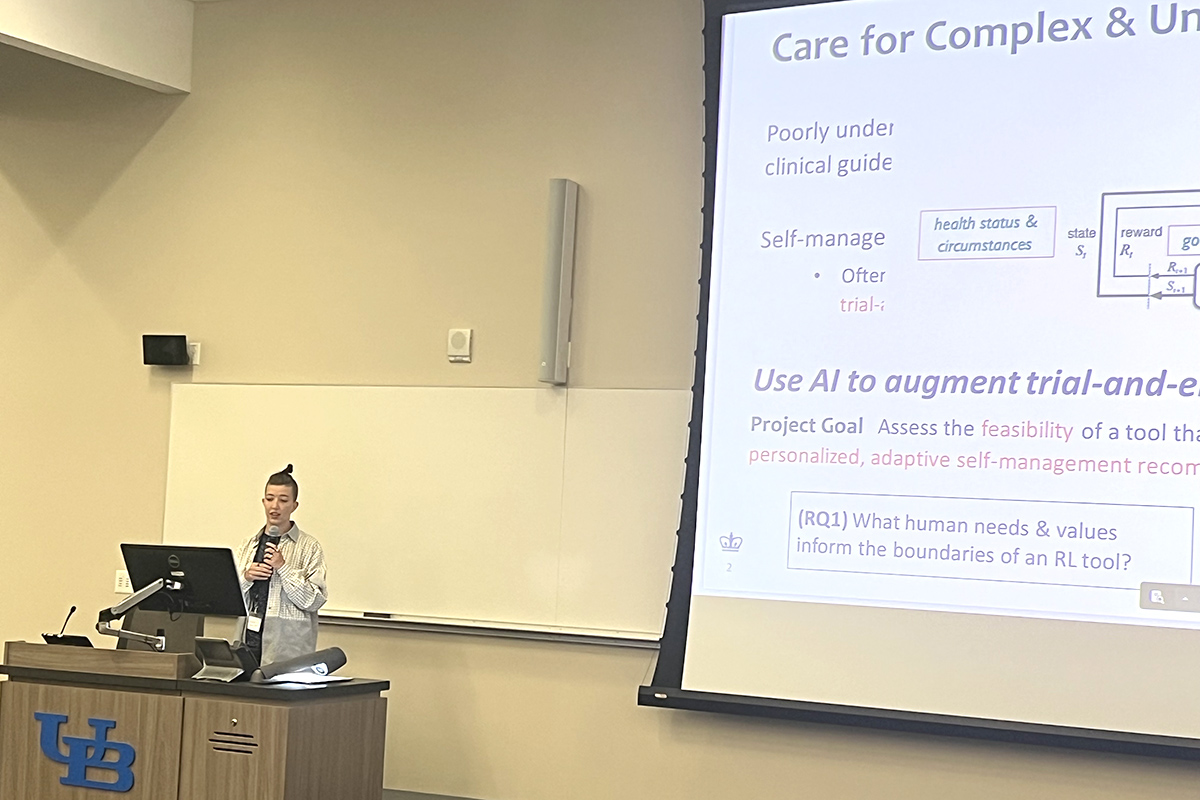
Compounding the challenge, chronic illnesses affect patients differently, requiring ongoing treatment and often a costly, time-consuming, and frustrating trial-and-error approach. Adrienne Pichon, PhD, explored ways to advance the development of more effective, personalized, and patient-centered technologies for managing complex chronic illnesses through human-centered artificial intelligence (HAI).

Adrienne Pichon, PhD
“Care for chronic illness is a major priority globally,” said Pichon, who recently completed her PhD in Biomedical Informatics at Columbia University. “It burdens healthcare systems and individuals alike, and it harms quality of life for those with one or more chronic illnesses. Chronic illness is complex and multifaceted, and people experience these diseases in very different ways.”
Endometriosis Presents Multi-Faceted Challenges
Endometriosis is a chronic condition affecting approximately 10% of women of reproductive age, characterized by unpredictable symptoms, a lack of biomarkers, no cure, and highly individualized treatment responses.
Before Pichon could design a system to empower patients in managing their care, she first needed to understand the obstacles they face. The first aim of her dissertation centered on qualitative research, using both interviews with endometriosis specialists and focus groups with individuals living with endometriosis.
“People talked about how complex endometriosis is in the different body systems that it impacts,” Pichon said. “It’s not just a reproductive condition or tied solely to menstruation. It can impact a vast array of body systems. Making sense of your illness and what is happening with your health is difficult, communicating that to providers is equally challenging.”
She found that while patients could describe how they felt in the moment, they struggled to convey the full scope of their symptoms over time. Many also found it difficult to communicate the different strategies they had tried to manage their symptoms.
“There are a lot of opportunities for intelligent systems to support individuals in their care tasks,” Pichon said.
 A Human-Centered Approach
A Human-Centered Approach
Human-centered AI (HAI) is designed to work alongside people, prioritizing human needs, values, and well-being by being transparent, fair, and user-friendly. Rather than a one-size-fits-all approach to treatment, Pichon aimed to build a one-size-fits-one system.
“Human-centered AI puts humans at the center of designing intelligent solutions, ensuring sure they align with individual needs and priorities,” she said. “AI should support the individuals. Humans need to do what they excel at, like using intuition and self-awareness, while they receive computational support from data science and machine learning.”
To achieve this, Pichon designed a framework called Multi-Perspective Directed Analysis (MPDA), which maps and aligns human needs with technical capabilities. Using Reinforcement Learning, the system provides adaptive self-management recommendations tailored to each patient. The goal is to generate personalized, explainable recommendations that benefit both patients and their clinical care teams.
“Adrienne’s research has the potential to shape patient-centered technologies that account for the individualized health status, needs, and circumstances of patients with chronic conditions,” said Noémie Elhadad, chair of Columbia’s Department of Biomedical Informatics and Pichon’s mentor. “Managing complex chronic illnesses is incredibly challenging, and this work could offer new solutions for patients who have long faced frustration in their health journeys.”
Elhadad’s Lab developed Phendo, an app designed to help individuals living with endometriosis to track and manage their condition, while contributing valuable data to advance research. Pichon used the real-world data from Phendo, as well as interviews and focus groups, to refine the framework. But Elhadad’s mentorship extended far beyond data access.
“Noémie helped me become an independent researcher,” Pichon said. “She asked tough questions and guided me toward answers, but she gradually removed supports along the way. As I enter the faculty job market, the ability to independently design studies, think critically about research questions, and assess real-world impact is invaluable.”
Next Steps Through Human-Computer Interactions
Pichon may have a new degree and a new title, but her work is far from over. Now a Postdoctoral Research Fellow in Lena Mamykina’s lab at DBMI, she continues to focus on informatics and human-computer interactions (HCI), with an emphasis on HAI to better understand how individuals navigate chronic illness.
A key aspect of her research will be integrating human narratives with self-tracked, machine-readable data to create meaningful health status representations. By combining rich, nuanced personal data with human expertise and control, she aims to develop intelligent systems that not only analyze health patterns but also reflect patients’ own perceptions of their well-being. This includes identifying the most relevant indicators of health status and improving how individuals communicate their experiences with providers.
Ultimately, her goal is to design systems that that bridge machine intelligence with human storytelling, enabling more personalized, effective, and patient-driven health management.